RPM: From Buried Data to $70k in Monthly Revenue
Role: Product Designer
How we designed a system that could automatically identify and bill insurance claims using complex remote patient monitoring data.
Key Impact
- $70,000 / month: In new, recurring revenue unlocked from the first month.
- Manual Process Automated: Replaced error-prone manual data review with a systematic workflow.
- Scalable for Growth: Designed to support business growth from 12 to 100+ clinics.
A Goldmine We Couldn't Access
At Enara, our entire model of care is built on continuous remote patient monitoring. Every day, our patients engage with us through the Enara app. Logging their weight from connected scales, sharing food pictures for feedback, tracking glucose levels, and chatting directly with their providers.
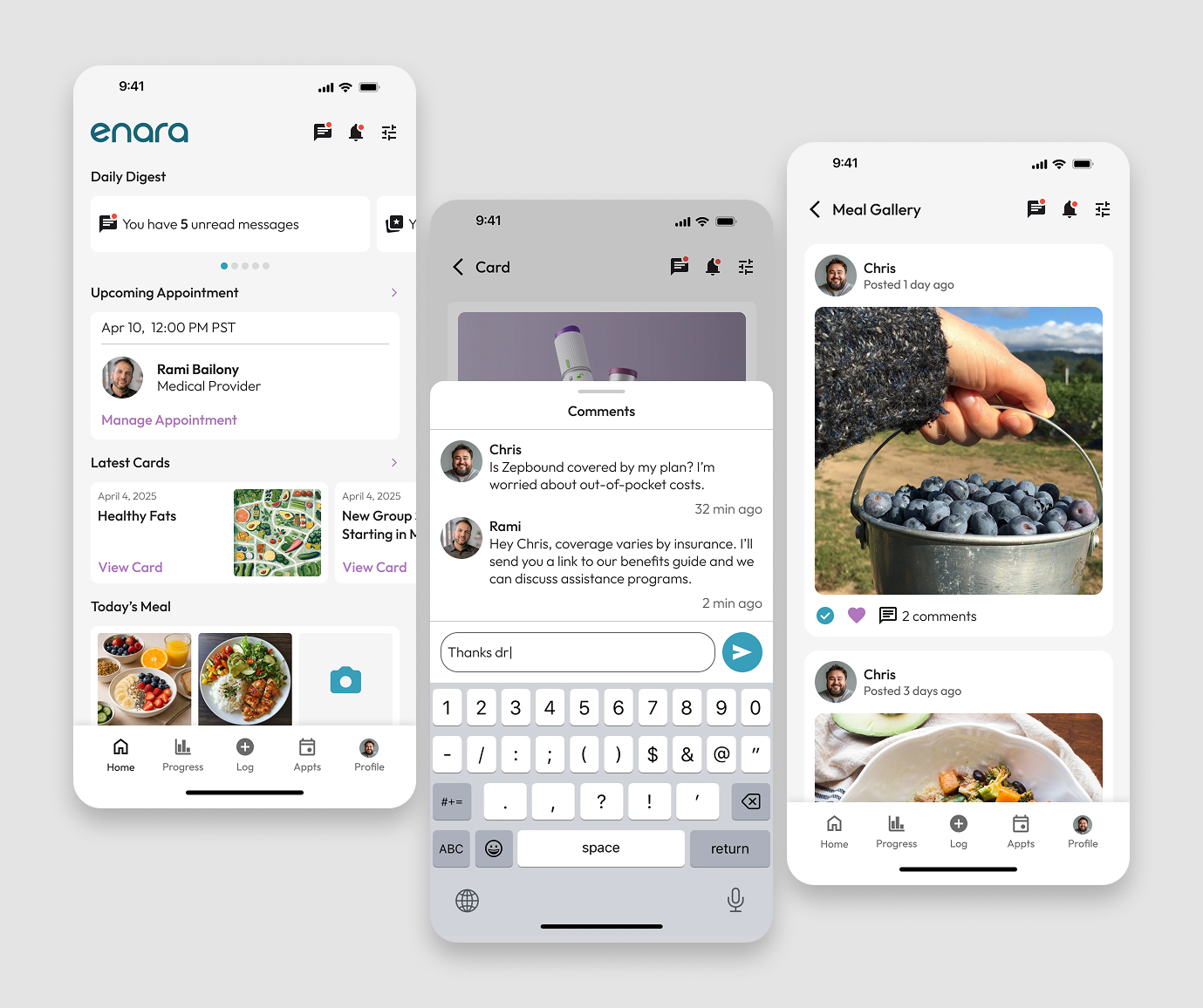
Each interaction is a valuable, billable event
This constant stream of data represented a goldmine of earned revenue. The problem? It was trapped. We had no systematic way to identify and process these thousands of daily micro-interactions into valid insurance claims.
Our billing team was forced to manually hunt for these claimable events, a chaotic process that was failing because of:
- Infinite Complexity: Every insurance plan has unique, shifting rules for what's billable.
- Manual Bottlenecks: Staff had to manually hunt through patient data to find billable events.
- Costly Errors: Incorrect codes and missed deadlines led to rejected claims and lost revenue.
- Inability to Scale: The entire process relied on tribal knowledge, making growth impossible.
The result was pure opportunity cost. Revenue we had earned through our care model but were unable to collect.
Build a Revenue Engine from Thousand of Daily Interactions
Messages, health tracking logs, and weigh-ins. Are the engine of our care model. But from a business perspective, their financial value was completely buried.
What can we actually bill for?
This project wasn't just about building a dashboard for our billing team. It was about ensuring the financial viability of our entire care model. The breakthrough was to reframe the problem from data visualization to signal detection. We needed an internal engine that could intelligently scan our stream of interactions, identify which ones qualified as billable care under complex insurance rules, and automatically package them for claims.
How we transform our billing team from manual data miners into expert validators.
The Solution: A Systematic Workflow for Revenue Recovery
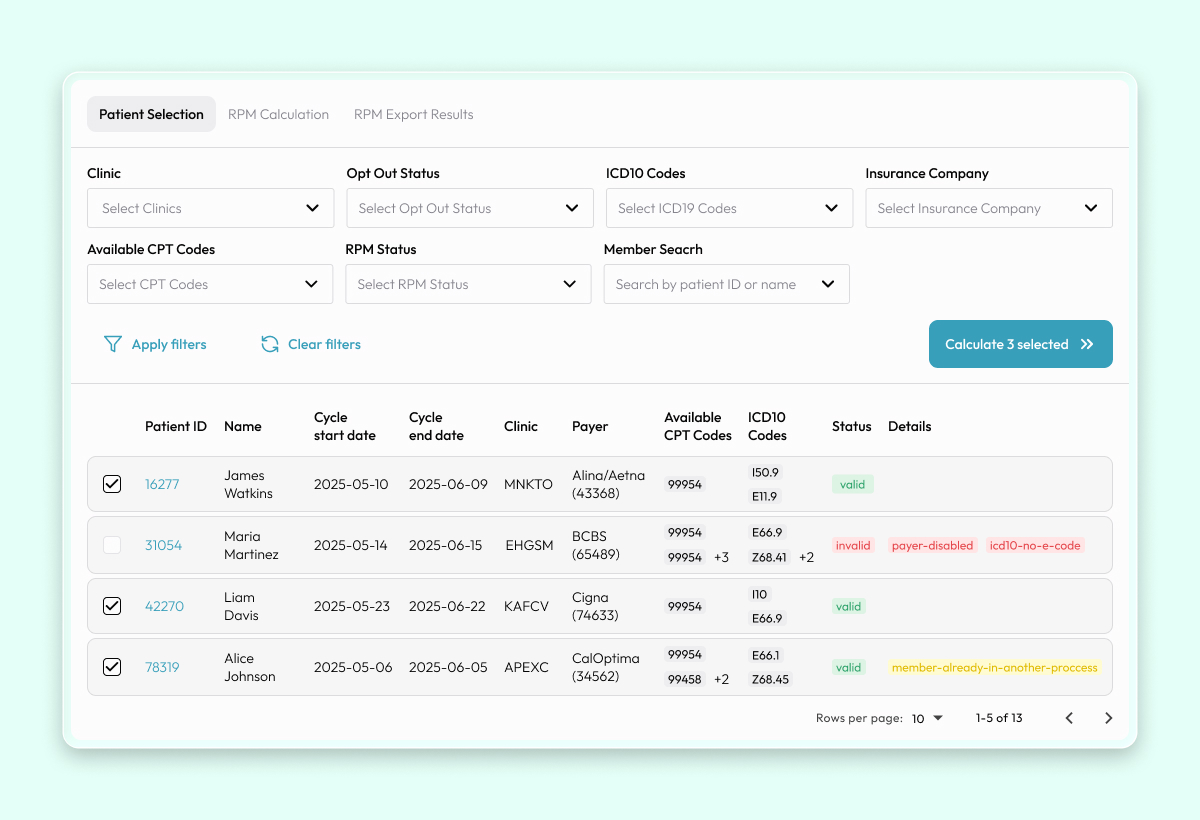
I designed a systematic, three-phase workflow that guides the billing team from raw data to validated claims with confidence and clarity.
Challenge 1: How do you tame the complexity of thousands of daily interactions?
Solution: A Guided, Multi-Step Process.
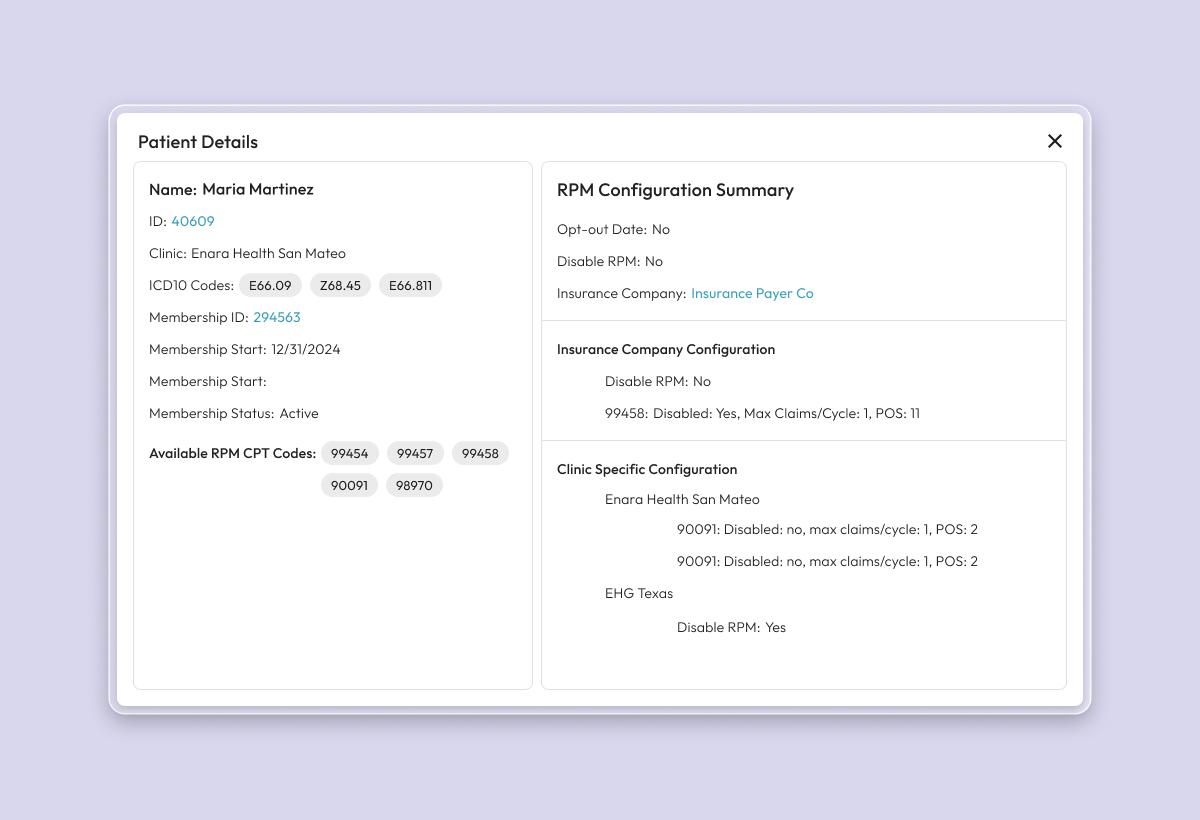
Instead of showing a raw feed of data, I designed a workflow that breaks the process into manageable steps: Select, Validate, and Export. The system automatically filters the stream of patient interactions and applies the correct, complex insurance rules during the validation step, surfacing only what is billable.
Challenge 2: How do you make financial data actionable for non-experts?
Solution: Make the Revenue Unmistakable.
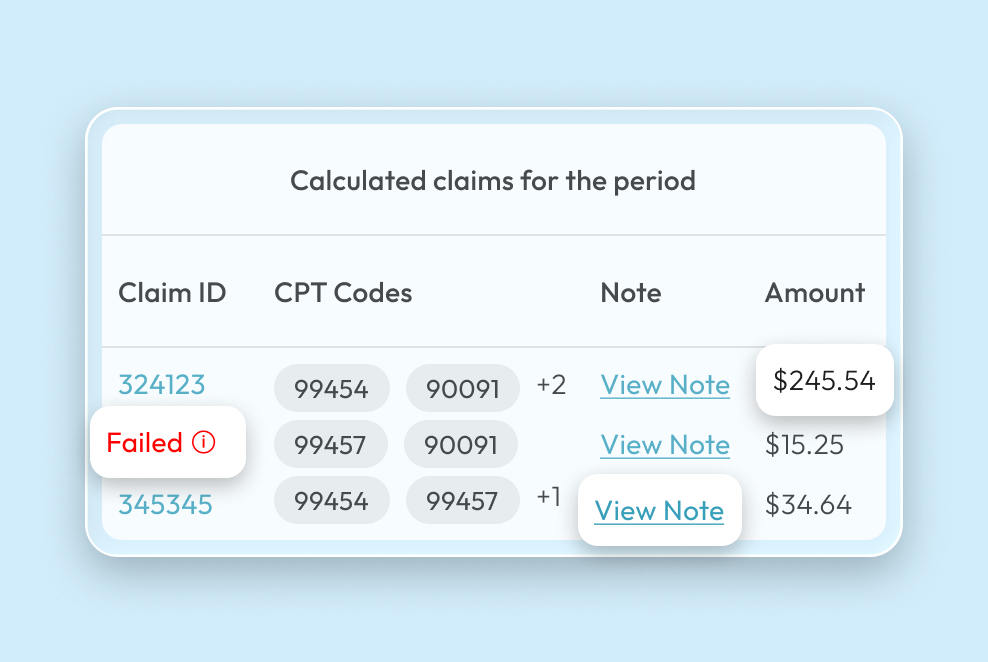
To empower the billing team to move quickly through thousands of potential claims, the financial impact had to be immediately clear.
- Clear Revenue Display: I designed the interface to show the exact dollar amount ($) for each potential claim.
- Actionable Error Messages: Instead of cryptic codes, errors were translated into plain English (e.g., "Payer Disabled," "Insufficient Codes").
- Simple Status Indicators: Clear, color-coded statuses (Valid, Invalid, Failed) removed all guesswork.
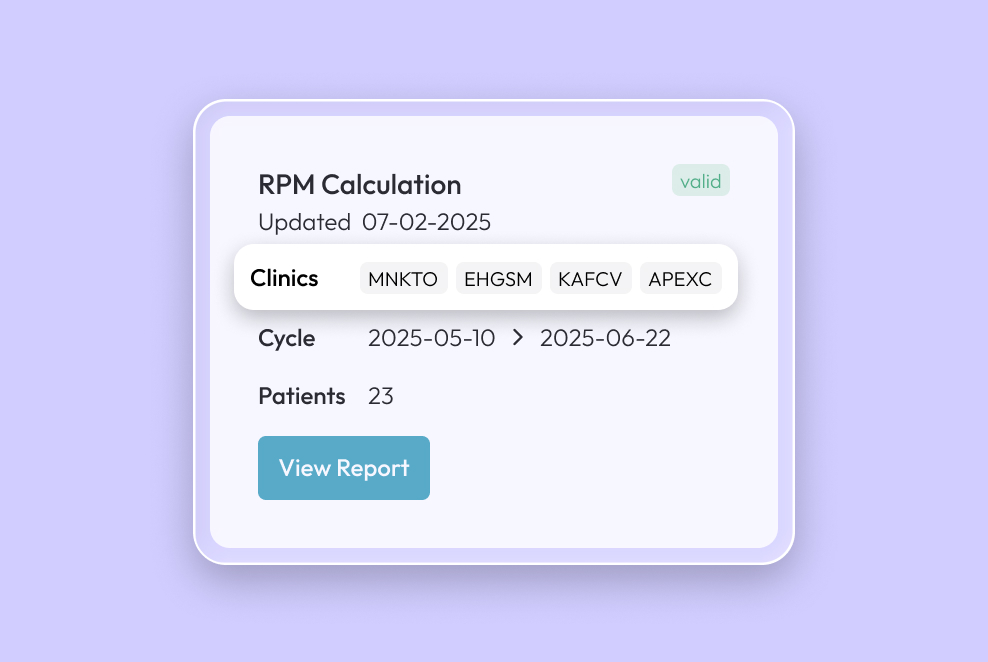
Challenge 3: How do you design for a business that needs to scale 10x?
Solution: Build for Tomorrow's Needs.
The system had to work for 12 clinics today and 120 tomorrow.
- "Airport-Style" Clinic Codes: I designed a simple, scalable abbreviation system (e.g., WMI, GCG) that was human-readable and could expand infinitely.
- Bulk Processing: The entire workflow was architected to handle hundreds of patients simultaneously without performance degradation.
A $70K Monthly Impact
The impact was immediate, transforming our ability to get reimbursed for the high-quality care we were already providing. It created a new, predictable revenue stream and fundamentally improved our operations.
- New Revenue Unlocked: $70,000 in the First Month
- Error Rates: ↓ Drastically Reduced through automated validation
- Team Efficiency: ↑ Significant Gains for the billing department
The billing team was no longer stressed and guessing. They were empowered, efficient, and directly contributing to the company's bottom line.
Takeaways
- In Healthcare, the System is the User Experience. Our solution had to connect three separate worlds: patient engagement tracking, clinical documentation, and complex insurance rules. I learned that you can't design for one part in isolation. A seamless interface is useless if the underlying system logic is flawed.
- RRevenue Follows Care, Not the Other Way Around. The biggest impact didn't come from focusing on money, but from understanding the entire patient journey. From a daily meal log to a paid insurance claim. When you design a system that supports high-quality care, revenue becomes a natural and sustainable outcome.
- Good Design is Evidence-Based. In a clinical setting, design decisions can't be based on opinion. I learned to ground my work in research, connecting interface design directly to the care factors that our own studies proved would lead to better patient outcomes. If the design doesn't support the clinical evidence, it's not the right design.
